Manchester scientists discover new “faster and more accurate” blood test for ovarian cancer
But funding is needed to save lives
Scientists at Manchester University have found a new way to test for ovarian cancer.
They say the new blood test has the potential to save lives - if further research can be carried out.
Professor Emma Crosbie, one of the researchers on the project, said:
“We do need to do something.
“It's all very well to say we are not diagnosing it early enough, but there has to be a willingness to try and do something about that.
“And that requires funders to put some money behind it.”
Ovarian cancer is currently diagnosed with a blood test, followed by an ultrasound scan.
But with a survival rate of just 35%, the current tests aren't picking up enough cases early enough.
The addition of a new type of blood test, developed by scientists at the University of Manchester, was 100% sensitive at detecting ovarian cancer in women under 50.
By using both the existing test and the new one in combination can pick up more cases of ovarian cancer more quickly than before - so people can access life-saving treatment faster.
“Anyone with ovaries can get ovarian cancer”
About ovarian cancer
From the NHS, “ovarian cancer affects the 2 small organs (ovaries) that store the eggs needed to make babies.”
While anyone with ovaries can get ovarian cancer (including trans men, non-binary people and intersex people), it mostly affects people over 50 and can run in families.
Your risk of ovarian cancer also increases if you:
- Inherited a faulty gene, such as the BRCA genes or those linked to Lynch syndrome
- Had breast cancer or bowel cancer
- Had radiotherapy treatment for a previous cancer
- Have endometriosis or diabetes
- Started your periods at a young age or went through the menopause late (over 55), or have not had a baby
- Have never used any hormonal contraception, such as the pill or an implant
- Are taking hormone replacement therapy (HRT)
- Are overweight
- Smoke
“An awful lot of women are diagnosed late”
Ovarian cancer survival rates
Despite being one of the most common cancers in women in the UK, ovarian cancer only has a survival rate of 35%, according to data from Cancer Research UK.
Compare this to other common cancers in women, such as melanoma skin cancer (the fifth most common, with a survival rate of 87%), breast cancer (the most common, with a survival rate of 76%), and uterus cancer (the fourth most common, with a survival rate of 72%), and you can see that much more research is needed.
Data from Cancer Research UK
“Early diagnosis is so important for ovarian cancer,” Alexandra Holden, deputy chief executive of the UK's leading ovarian cancer charity Target Ovarian Cancer tells us, “it is absolutely crucial, and it really does change the life chances of an individual to be diagnosed early.
“Unfortunately, an awful lot of women are diagnosed late and of course, that means that their prognosis is not as good.”
According to Crosbie, who is also a gynaecological cancer surgeon: “Survival drops off terribly as you go from stage one to two to three to four.
“In general, in the UK, we're picking up mostly stages three and four.”
She explains that this is partly because “at the moment, what happens is, ovarian cancer presents quite late. So it usually presents at an advanced stage, and the outcomes are quite poor.”
“Partly this is because we think that there is somewhat of a delay between patients noticing that they've got symptoms, the GP noticing that those symptoms could be ovarian cancer and them doing the tests that then allow them to access further tests and secondary care.”
“Neither brilliantly sensitive nor brilliantly specific”
Current diagnostic tools
Doctor Garth Funston, another of the researchers and himself a GP, said that when people present with the symptoms of ovarian cancer, they will then be given a blood test, Cancer Antigen 125 (CA125), which has been used for many years but fails to pick up “around 15%” of ovarian cancer cases.
Crosbie says that this is because CA125 is “neither brilliantly sensitive nor brilliantly specific.”
After the CA125, they will be referred for an ultrasound scan.
“It's this combination of having a high CA125 and an abnormal ultrasound scan,” Crosbie tells us, “that then makes us think, ‘this patient might have ovarian cancer’.”
“Women don't want to be a burden”
Getting an ovarian cancer diagnosis in the UK
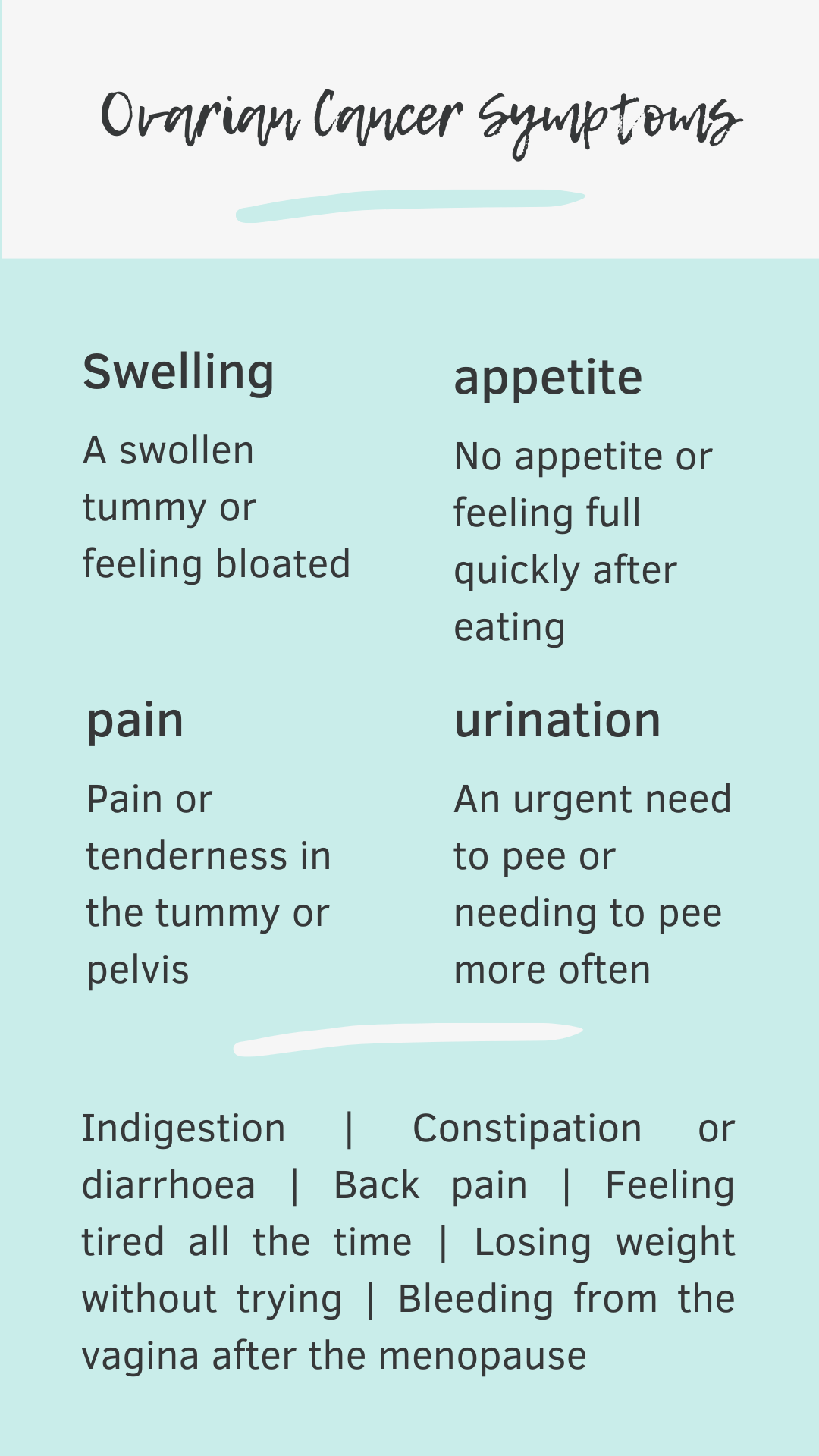
Holden tells people to look out for four key symptoms of ovarian cancer: persistent bloating (not bloating that comes and goes through the month), difficulty eating (and feeling full really quickly), abdominal pain, and needing to wee more often (and more urgently) than usual.
The NHS lists other common symptoms of ovarian cancer as:
- Indigestion
- Constipation or diarrhoea
- Back pain
- Feeling tired all the time
- Losing weight without trying
- Bleeding from the vagina after the menopause
Unfortunately, these symptoms are both very nonspecific and very common.
“The difficulty with diagnosis of ovarian cancer,” Holden says, “is that most women are diagnosed over the age of 50, which is when women are experiencing a lot of changes in their body, menopause, those types of things.
“A lot of women will then put it down to just getting older, or their body changing and therefore not notice that these things are happening.”
As well as not always knowing what symptoms to look out for, part of the issue with diagnosing ovarian cancer, Crosbie tells us, is that women “don't want to be a burden, so they’ve noticed something but they don't think it could be anything serious, and they don't want to be seen to be mithering their GP.”
“Over 1,000 women of Manchester”
The Manchester Connection
The research study was carried out at Manchester University with funding from Wellbeing of Women, an organisation that improves the health and wellbeing of women, girls and babies through research, education and advocacy.
Researchers used blood samples from over 1,000 women of Manchester.
There is a disparity in rates of ovarian cancer based on what region people live in.
Looking at the most recent ONS figures, London has the lowest rates and the North East the highest, with the North West another of the hardest-hit regions of England.
“It's really the addition of another blood test”
The science part
In the past, the focus in cancer research has been on trying to improve treatments - which is obviously important.
But, Crosbie tells us: “if we're going to make appreciable differences to women with ovarian cancer in terms of prolonging their survival, we need to be doing things about diagnosing it earlier.”
That’s where the study comes in.
Dr Funston describes it in a nutshell: “We looked at whether adding another blood test, and that's HE4, could improve the detection of ovarian cancer,” he explains, “it's really the addition of another blood test and we also looked at it within an algorithm as well.”
Here is Professor Emma Crosbie explaining the research in more detail.
Audio Explainer: New blood test for ovarian cancer
With Professor Emma Crosbie
“We basically wanted to see if there is any way of improving referral of women with symptoms suggestive of ovarian cancer from primary care to secondary care for tests.
“So we wanted to know whether, you know, we could improve on that sort of referral.
“So getting the right people in through the door in terms of not missing anyone who potentially has ovarian cancer.
“But also trying to reduce the number of healthy women who have an abnormal CA125 and who then actually don't have anything wrong with them
“Because CA125 is neither brilliantly sensitive, nor brilliantly specific.
“So we measured not just the CA125 which was being done routinely, but we added in another blood test called HE4, which is another biomarker that's been looked at that might have some promise for ovarian cancer detection.
“And then we had a look to see whether or not that combination of CA125 and HE4 could in fact improve the diagnostic accuracy of referring women for a scan.
“And we were able to look then at how many would CA125 on its own pick up?
“How many would HE4 pick up?
“And if we did them together, how many would that pick up and how many would it exclude?
“And then we looked at women on the basis of age because we know that CA125 can be raised in premenopausal women with benign conditions like endometriosis, and we know that HE4 can be raised as people get older.
“And we actually found that if you do add in HE4 that can be really, really helpful in terms of not missing anybody in the premenopausal group that would have ovarian cancer.
“So it was 100% sensitive, the combination of HE4 and CA125 in a calculation called ROMA, which is a Risk of Ovarian Malignancy Algorithm.
“And in postmenopausal women, it wasn't quite as good, but adding in HE4 did improve the accuracy slightly of CA125.
“There's a trade-off between sensitivity and specificity.
“So as you capture more people, you risk doing lots of tests on people who are normal and the harm that can cause and the costs that that generates.
“It might well mean that we see more patients at hospital for a scan, because it's going to refer more patients through in order to not miss any.
“So it's not perfect in the sense that it doesn't simply pick up people with ovarian cancer, it also picks up a whole load of other people who don't have ovarian cancer.
“So it will reduce the number that are reassured in GP, increase the pool of women coming through for a scan, but also therefore reduce the number that are undiagnosed.
“And I guess it's about where you draw that sweet spot, you know, what is an acceptable number of women to be investigating to find the patient with ovarian cancer?”
“A glimmer of hope”
What the study could mean for people with ovarian cancer
Dr Funston said of the study: “The idea is that it can help pick up more cancers, help women be diagnosed more quickly, and start treatment more quickly, which could help improve outcomes such as survival.”
But, when asked how soon this testing might be accessed by GPs and the general public, he warned that “it's likely years, unfortunately, to do things properly and safely.”
Holden is familiar with the slow progress of ovarian cancer research: “With just over 7000 women diagnosed each year it just takes a bit longer to research and to get those people through trials because there's less people to get the data from.”
“The bottom line,” according to Professor Crosbie, “is that probably CA125 on its own is not good enough, and that something like HE4 can help.
“Ultimately, we need more research in this space because we're still doing really badly with picking up ovarian cancer.
“But for us to now introduce that into the NHS, I think we would need to have a larger prospective study.
“It needs to be a massive, massive study.
“Logistically that's quite challenging and also obviously very expensive to do.”
But she remains positive: “Our study was really just quite a small study, but it showed a glimmer of hope. ”